Components
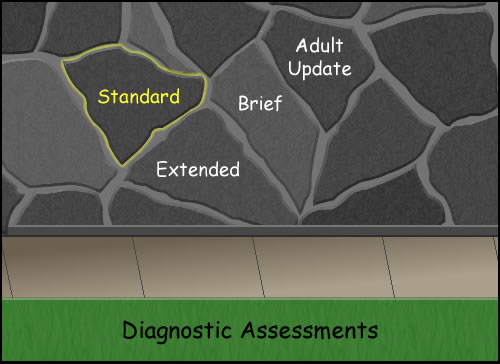
The Diagnostic Assessment Report has components that correspond to the following areas.
Click on each to learn more.
The components under client's current life situation include:
Click on each to learn more.
- Age.
- Current living situation, including household membership and housing status.
- Basic needs status, including economic status.
- Education level and employment status.
- Significant personal relationships, including the client’s evaluation of relationship quality.
- Strengths and resources, including the extent and quality of social networks.
- Belief systems.
- Contextual non-personal factors contributing to the client’s presenting concerns.
- General physical health and relationship to client’s culture.
- Current medication.
There are also required components that fall under reasons for the assessment.
Click on each to learn more.
- Description of symptoms including reason for referral..
- Client’s perception of his or her condition.
- History of mental health treatment including review of records.
- Developmental incidents.
- Maltreatment or abuse.
- History of alcohol and/or drug use/abuse.
- Health history and family health history.
- Cultural influences.
The mental status exam (MSE) is a structured way of
observing and describing a client’s current state of mind.
It typically includes the domains of:
- Appearance
- Attitude
- Behavior
- Mood and affect
- Insight and judgment
- Speech
- Thought process
- Thought content
- Perception
- Cognition
Assessment of client needs is based on the following six areas.
We will explore these on the next screens.
- Baseline measures
- Symptoms of behaviors
- Skills and abilities
- Resources
- Vulnerabilities
- Safety needs
Assessment of client needs is based on the following six areas.
Baseline Measurements
Comparing or compiling information of an individual’s mental health symptoms and their impact on functioning are the key to not only measuring the outcomes of treatments on a broad scale, but crucial to the clinician's full understanding of patient's individual needs.
Symptoms of behaviors
Behavior is an action or reaction to the environment or to internal thoughts and emotions. Behavioral symptoms are persistent or repetitive behaviors that are unusual, disruptive, inappropriate, or cause problems.
Skills and abilities
What unique aptitudes and talents do the individual have that may influence the recovery and reliance for an individual? These may include skills such as reading or writing or problem solving or decision-making skills. Or they may include skills such as being able to manage time or money.
Assessment of client needs is based on the following six areas.
Resources
Where does the individual receive support or aid and are there resources that they are able to readily draw upon if needed? These can include personal resources or professional resources.
Vulnerabilities
These include areas where the individual is susceptible to physical or emotional injury or attack. These may include an individual’s susceptibility to manipulation, persuasion, temptation, etc.
Safety needs
Safety needs can include vulnerabilities, suicidal thoughts/actions, and self injurious behavior (SIB)
The mental status exam (MSE) is a structured way of
observing and describing a client’s current state of mind.
Screenings used to determine substance abuse, and other standardized screening instruments.
At this time substance use/abuse screenings are the only required screening.
Access required screening tools on the
Integrated Treatment for Co-Occurring Disorders website. More information about substance screening tools will be covered in chapter 10.
Assessment methods
There are additional assessments currently required for DA’s completed for a child. Please note that these need to be put into the MN-ITS system.
Use the following links for more information.
- View the Child and Adolescent Service and Intensity Instrument (CASII) that helps determine the
service needs of children and adolescents. - Access the Early Childhood Service Intensity Instrument (ECSII) that focuses on the service needs of
infants, toddlers, and children from ages 0 to 5 years in the context of their families and communities. - View the Strengths and Difficulties Questionnaire (SDQ) that is used for 3 to 16 year olds to detect
their general symptoms and development assets.
The following is a list of component items under the clinical summary:
- Recommendations
- Prioritization of needed mental health, ancillary, or other services
- Client and family participation in assessment
- Referrals to services required by statute or rule
- Service preferences
- Cause, prognosis, likely consequences of symptoms
- How Dx criteria is met: symptom, duration and functional impairment
- Strengths, cultural influences, life situations, relationships, health concerns and how Dx
interacts/impacts with the client’s life - Explain R/O, other provisional Dx, and why alternative Dx that were considered were ruled out
Diagnosis on all Five Axis:
Axis I: Clinical disorders, including major
mental disorders, learning disorders and substance use disorders.
Axis II: Personality and intellectual disabilities
Axis III: Acute medical conditions and physical
disorders
Axis IV: Psychosocial and environmental factors contributing to the disorder
Axis V: GAF (Global Assessment of Functioning) or Children’s Global Assessment Scale
Print the Diagnostic Assessment Report.